Shocking Drop in U.S. Life Expectancy: COVID-19’s Devastating Impact Revealed
The emergence of COVID-19 five years ago marked one of the most severe public health crises in modern history.
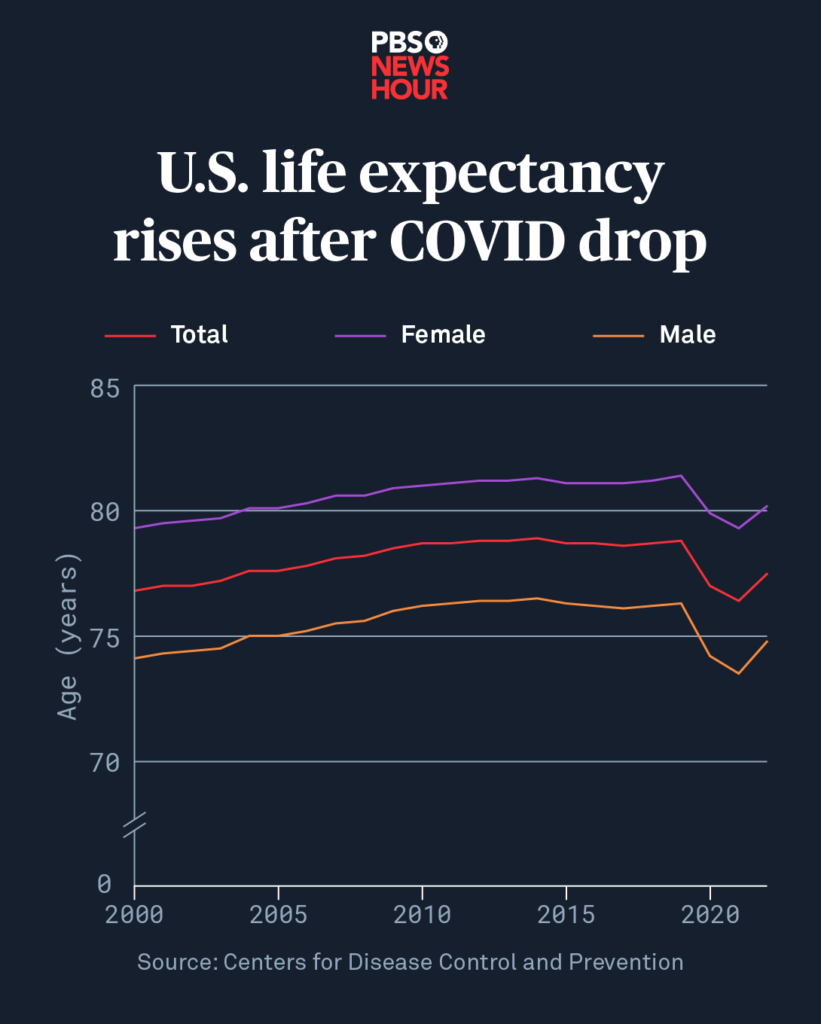
Five years ago, the outbreak of COVID-19 rapidly evolved into one of the most severe public health emergencies in modern history, profoundly affecting populations across the globe. In the United States, the pandemic’s impact was particularly devastating, with life expectancy plunging by approximately 2.7 years during its first two years alone. This dramatic drop marked the sharpest decline in U.S. life expectancy since World War II, underscoring the widespread toll the virus has taken on public health.
A significant factor contributing to these troubling statistics has been the interplay between COVID-19 and heart disease, a condition that has long been the leading cause of death both in the U.S. and worldwide. The pandemic intensified the effects of cardiovascular disease, as COVID-19 infections often worsened pre-existing heart conditions and triggered new complications in vulnerable individuals. As a result, deaths related to heart disease surged during the pandemic, further magnifying the public health crisis.
The Rise in Strokes and Blood Clots
The SARS-CoV-2 virus, which causes COVID-19, has been linked to an increased risk of dangerous blood clot formation throughout the body. This heightened clotting activity can lead to life-threatening complications such as strokes, deep vein thrombosis (DVT), and pulmonary embolisms. As the virus spread rapidly, these severe health issues became more frequent, placing immense pressure on already overwhelmed healthcare systems. Hospitals faced rising numbers of patients requiring urgent care for clot-related emergencies, further contributing to the overall surge in mortality rates during the pandemic.
The Opioid Epidemic and Spike in Overdose Deaths
While the COVID-19 pandemic unfolded, the United States was already grappling with another major public health crisis: the opioid epidemic. The stress, isolation, and limited access to support services during pandemic lockdowns intensified substance use issues, leading to a dramatic increase in opioid-related fatalities. The widespread availability of synthetic opioids like fentanyl only worsened the crisis, with overdose deaths reaching record highs. By 2022, unintentional injuries—primarily driven by drug overdoses—had become the third-leading cause of death in the U.S., highlighting the devastating overlap of these two health emergencies.
Alcohol Use and Rising Liver Disease Cases
The COVID-19 pandemic brought widespread social isolation, heightened stress levels, and significant disruptions to routine healthcare services, all of which contributed to an increase in alcohol consumption across the United States. Many individuals turned to alcohol as a coping mechanism during lockdowns, leading to a surge in heavy drinking and alcohol dependency. This rise in alcohol misuse, combined with limited access to preventive care and treatment for substance abuse, significantly worsened liver health nationwide.
Liver disease, particularly alcohol-related liver conditions such as cirrhosis and alcoholic hepatitis, became more prevalent during this period. Delayed medical interventions and the progression of undiagnosed cases further compounded the issue. As alcohol consumption and liver-related complications continued to rise, these factors contributed to a noticeable decline in overall life expectancy, underscoring the pandemic’s far-reaching effects on public health.
Temporary Decline in Respiratory Disease Deaths: A Brief Silver Lining
While the COVID-19 pandemic caused widespread devastation, there was a temporary decline in deaths from certain respiratory illnesses, providing a brief silver lining amid the crisis. Preventive measures such as social distancing, mask-wearing, and increased hand hygiene—implemented to curb the spread of the coronavirus—also proved effective in reducing the transmission of other respiratory infections like influenza and respiratory syncytial virus (RSV). These illnesses, which tend to disproportionately affect vulnerable populations such as infants, young children, and the elderly, saw a significant drop in cases and fatalities during the height of pandemic restrictions.
However, as public health measures were gradually lifted and life returned to normal, infections from these seasonal viruses surged once again. With weakened population immunity due to limited exposure during lockdowns, the resurgence of flu and RSV led to a renewed strain on healthcare systems, amplifying the pandemic’s lasting impact on public health.
Declining Mortality Rates and Emerging Long-Term Health Concerns
By the fourth year of the COVID-19 pandemic, mortality rates began to decline gradually across the United States and many parts of the world. This positive trend was largely driven by the widespread rollout of vaccines, which significantly reduced severe illness and death, along with increased population immunity from both vaccination and prior infections. However, while the immediate danger from COVID-19 infections subsided, the virus’s long-term health consequences have continued to surface.
A growing body of research has linked COVID-19 infections to lingering health complications, such as an increased risk of dementia, cardiovascular issues, and developmental delays in children. These long-term effects serve as a sobering reminder that, even as society attempts to move forward, the virus’s impact persists. The pandemic has left a lasting imprint on global health and longevity, with its consequences expected to influence public health outcomes for years to come.


Comments are closed, but trackbacks and pingbacks are open.