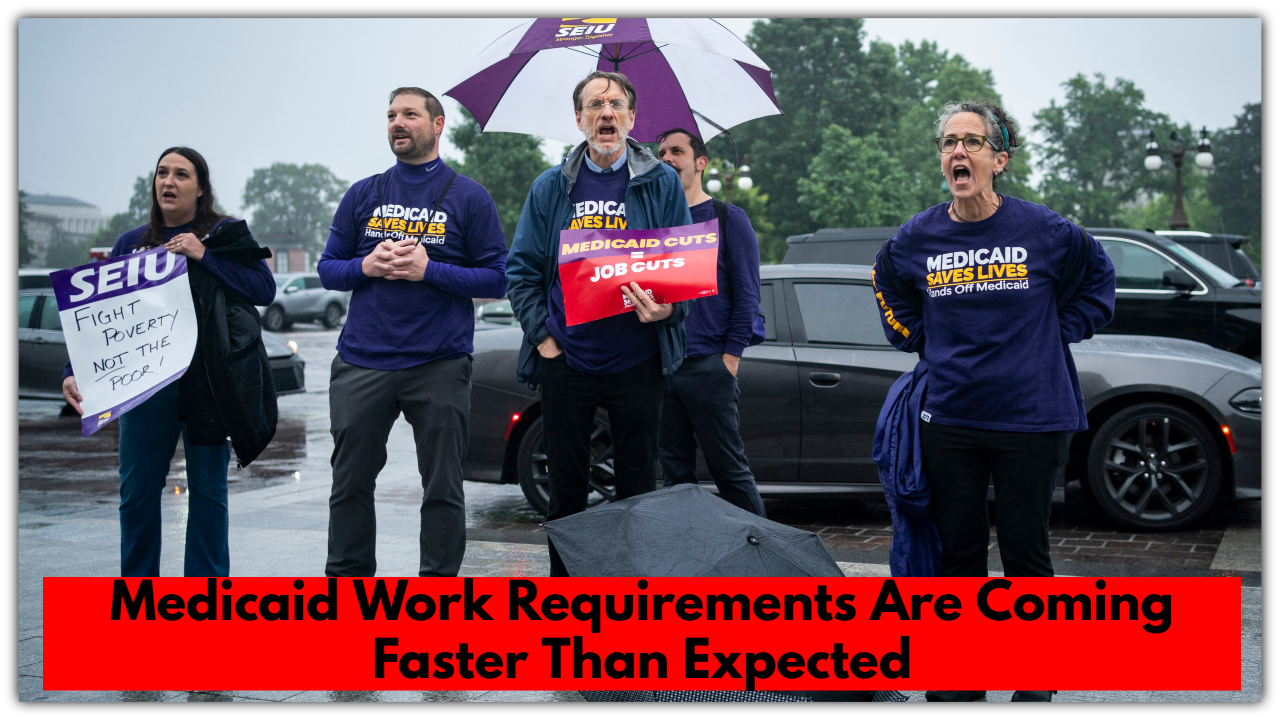
Medicaid Work Requirements Are Coming Faster Than Expected—Are You Ready?
There’s a big change brewing in how Medicaid works, and it’s happening faster than expected. Congress just gave the green light to a bill—yes, seriously called the “One Big Beautiful Bill”—that would move up the start of Medicaid work requirements to December 2026. That’s a full two years earlier than originally planned.
So what does that mean for everyday people? Let’s break it down in plain English.
What Are Medicaid Work Requirements, Anyway?
If you’re an adult who gets health coverage through Medicaid (especially under the Affordable Care Act), you may soon have to prove that you’re working—or doing something similar—for at least 80 hours a month to keep your insurance.
That “something similar” could include things like job training, going to school, volunteering, or doing community service. It’s not just about holding a traditional 9-to-5.
There are some important exceptions. If you’re:
-
Over 65
-
Disabled
-
Pregnant
-
Taking care of someone full time
…then you wouldn’t have to meet these work requirements.
But for a lot of people, especially those juggling part-time jobs, family responsibilities, or irregular work schedules, this could be a pretty big shift.
Why the Rush to Start in 2026?
It all comes down to politics and money.
The lawmakers pushing this bill say moving up the timeline will help the government save money—possibly more than $280 billion. The idea is that fewer people on Medicaid (especially those who can’t keep up with the new rules) means lower costs for the program overall.
That’s appealing to some politicians. But others are sounding the alarm, saying the real cost might be people’s access to health care.
What Could Go Wrong?
A lot, actually—and it’s not necessarily about people refusing to work.
The truth is, many of the people who could lose coverage are already working. But they might lose Medicaid simply because they missed a deadline, couldn’t figure out how to report their hours, or got caught in red tape. Think about folks who don’t have internet access, work irregular hours, or don’t speak English fluently. It’s easy to slip through the cracks in a system like this.
The government’s own numbers back this up. A recent estimate says over 10 million people could lose Medicaid coverage by 2034. And half of that would be directly tied to these new work rules—not because people aren’t working, but because they struggle to keep up with the reporting process.
Where Things Stand Now
So far, this bill has only passed in the House of Representatives. It still needs to get through the Senate and be signed by the President before it becomes law. That could happen as soon as this summer.
And while that’s being debated, some states—like Arkansas, Ohio, and Arizona—aren’t waiting. They’re already pushing ahead with their own versions of these work requirements.
Why This Matters
If you or someone you love relies on Medicaid, this is something to pay attention to. Because while the idea of requiring work might sound fair on paper, in real life, it’s way more complicated.
People are busy. Life is messy. And adding another layer of paperwork or digital reporting can be overwhelming—especially for folks already dealing with unstable jobs, family care, health issues, or just trying to make ends meet.
This change could mean a lot of people lose their health coverage—not because they’re lazy or unwilling to work, but because the system asks them to jump through hoops that aren’t built for real life.


Comments are closed, but trackbacks and pingbacks are open.